Haley H.
- Author: Haley H.
- Date Submitted: Jun 14, 2021
- Category: COVID Rehab


“I had no symptoms. None of the signs that people usually complain about with COVID. No fever, no cough, no fatigue. I guess that’s why they never thought about it when I went into the hospital the first time.”
That’s 23 year old Haley from Barnesville speaking about her experience of COVID-19. We met her at Allied Services Wilkes-Barre Rehab Hospital. She was admitted to the inpatient rehabilitation hospital after experiencing stroke-like symptoms as a result of the virus.
Haley had no warning of her illness. She simply collapsed while getting ready for work one day.
“I was just going about my morning routine. Nothing felt out of the ordinary. Then my Mom found me passed out on the bathroom floor. She got me up and asked me if I was ok. I said yes and she was helping me back to my room when it happened again. She yelled for my Dad and they took me to the hospital.”
At the local emergency room, doctors could not find anything immediately wrong despite extensive testing. Haley was discharged and advised to follow up with her family doctor and a cardiologist.
“As we were leaving the ER, my speech and walking started to go. My speech sounded like I had been drinking all day, and as it progressed, I couldn’t walk without help. I had to have both my Mom and Dad on each side of me, and even then it was still hard to walk. Later that morning, they took me back to the hospital and this time they did a CT Scan, an MRI, and a COVID test. The COVID test came back positive. The CT Scan was normal, but the MRI showed my Cerebellum was inflamed.”
The cerebellum is a dense, fist-sized formation located at the base of the brain that plays an important role in motor control. In particular, it is active in the coordination, precision, and timing of movement. The cerebellum also plays a role in eye movement, motor learning, and fine-tuning. It is also believed to play a role in some language and mood processing, however, these findings are yet to be fully verified.
Haley underwent testing at St. Luke’s in Orwigsburg including a spinal tap. The results of the spinal tap and other labs could do nothing to explain her ongoing symptoms. With no improvement in her health, Haley sought help at Penn State Hershey Health Center.
“They did another CT Scan, another MRI, and more x-rays. The x-rays showed I had pneumonia. You wouldn’t even know I had pneumonia or COVID. I had no signs of either. No fever, no cough. Nothing! The MRI showed the swelling in my cerebellum had gone down so they started me on Remdesivir for 2 doses and steroids for the rest of the time I was there until I came here, to Allied.”
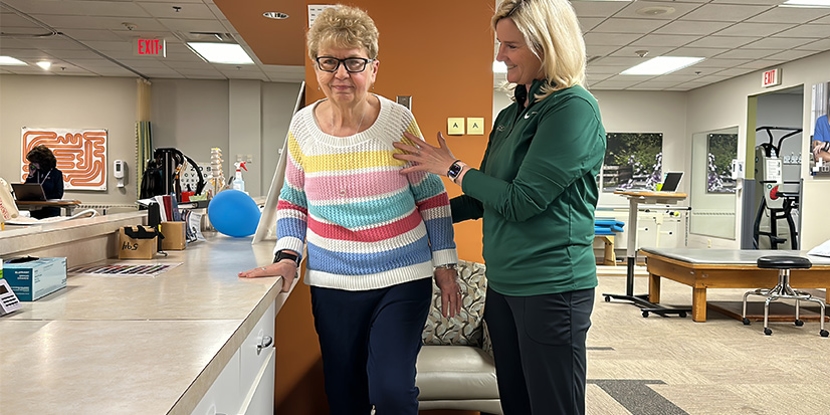
When Haley arrived at Allied Services Wilkes-Barre Rehab Hospital she met was met by a team of nurses and therapists all specially trained in rehabilitation medicine.
“Haley had poor trunk control; poor control of her hips; poor control of her legs. She was very ataxic on evaluation, and like we see in individuals with COVID… she would fatigue very easily, especially in her legs. However, atypically, she is making a turnaround very quickly” noted Walter Slivinski, PT, DPT.
Haley’s therapy team designed a treatment plan designed to restore function necessary for her to return home, and eventually, return to her job as a scientist. The physical therapy team worked to steadily build Haley’s strength, increasing the complexity and difficulty of the activities to challenge both her cognitive and physical abilities.
“She doesn’t get as tired as she used to and we are able to do more and more with each session. Her legs get tired, but that’s because that’s where we are challenging her. When she leaves here and goes home, and then to outpatient therapy; eventually she wants to return to work and her job requires her to stand for multiple hours a day. Getting back to that normalcy is important to her.” Walter Slivinski, PT, DPT.
“Because Haley is a Scientist in a lab we’ve been working on the fine motor coordination and strength in both her hands to improve function so she can get back to work” says Patricia Lepore, OTR/L. “We simulated her use of tweezers, a pipet, and test tubes. We incorporated those with her standing balance to improve her standing tolerance for when she is back to work. Her energy level, pure determination and motivation to return to work really sparked our therapy sessions.”
The swelling in Haley’s brain did not cause any permanent damage however, like an injury to any part of the body the inflammation caused irritation to the surrounding tissues and nerves which resulted in some of Haley’s lasting symptoms.
“The best way a doctor described it to me was it’s kind of like I had a stroke without actually having a stroke. I couldn’t walk or sit right. Controlling my hands and arms was difficult. For a while I talked like I had a stroke, but my brain didn’t suffer any of the permanent damage that a stroke would cause. Now that the swelling is going away, I’m getting stronger and things are getting back to normal” says Haley.
“Someone asked me to describe how I felt and if I was ever in any pain - and I never had any pain - or numbness. For people a bit younger like myself, I tell them that I felt like I was always in a bounce house; that feeling of always being off-balance or having Jell-O legs.”
“Haley is the youngest person I’ve worked with affected by COVID, so for me, it was like working with my daughter especially since they went to the same college. But to see somebody so young have the deficits that she had, to be as unstable as she was - it was really eye-opening. We haven’t seen that here with anyone with COVID. We’ve seen the respiratory issues, we’ve seen the de-conditioning, but we haven’t seen these neurologic effects. So she has opened my eyes to see that maybe others that have COVID may be suffering these neurologic impacts that we just aren’t seeing or are possibly being masked or labeled as something else” noted Walter Slivinski.